Expert Services
You need and deserve expert and compassionate care. At Pisacano Eye, your vision is our number one priority and we believe you should be treated like family. We take that statement very seriously— after all, Pisacano Eye is a professional, family-owned and family-staffed eye care practice

Services
EYE EXAMS
Scheduling a routine eye exam with your eye doctor is important to maintain your eye health and vision. While people are often more prone to reach out to their eye doctor when there are issues with their eyes, we encourage all patients to schedule an eye exam regularly to ensure that your eyes remain healthy. Many eye diseases out there have little to no warning signs until it is too late. Please consider scheduling your next eye exam appointment with us, so our professional eye doctors can check the overall health and vision of your eyes. There are a few leading diseases that can cause blindness in people: The eye diseases listed above are a few of the common illnesses that can cause blindness without showing any early signs or symptoms. That is why we encourage all our patients, for their safety, to have a comprehensive eye exam routinely to ensure the health of your eyes. Wondering when you should schedule an eye exam and how often they should be? We recommend that children have their first eye exam that includes a measurement of their vision, before they enter kindergarten. After this, their vision should be measure every few years to ensure their eyesight is developing normally. Teenagers should have a full eye examination before they begin driving. Adults should have a comprehensive eye exam every year or two starting at the age of 40. After age 50, it is highly recommended to have an eye exam every year, as eye diseases that cause blindness become more common. There are a few exceptions to this standard, however. Those who have diabetes should have an eye exam each year after their diagnosis, no matter the age. Those who have close relatives that have developed eye diseases should also have eye exams every year from age 30 and older. For those diagnosed with diabetes, regular eye examinations are important in order to ensure that diabetic eye disease and the vision lost cost by it can be prevented. In diabetes, high sugar levels in the blood cause damage to the blood vessels throughout the body. Our eyes have many blood vessels that supply nutrients to it. Uncontrolled diabetes can affect our eyes as the constant elevated sugar levels can target the various blood vessels found in our eyes, specifically, the retina. Since the retina is responsible for light detection and sending signals to our brain to perceive what we see, once these blood vessels are damaged our vision can definitely be compromised. Over time, the blood vessels in the retina develop weak spots due to the damage they have incurred. These weak spots expand, almost bubble-like, along the blood vessels, making them microaneurysms. If these microaneurysms rupture, blood will then fall into the retina and create small dot hemorrhages. The retina has the ability of clearing the blood away, but often debris is left behind which hardens and progresses to being hard exudates. These three changes, microaneurysms, small dot hemorrhages and hard exudates, are referred to as background diabetic eye disease. Those who have had diabetes for 10 or more years often experience this. Occasionally, these changes can progress to increases hemmhorages and swelling in the center of the retina, called the macula. More often than not, this will cause some degree of vision loss. All these changes fall under the category of background diabetic retinopathy. Because of these various changes and compromise to the existing blood vessels, our brain instructs the retina to grow new blood vessels in order to make up for the deficits of blood supply. However, because of the lack of space, the retina will attempt to grow new blood vessels to replace the broken ones, often in the wrong places. These new growths are called proliferative diabetic eye disease. These new blood vessels are very fragile and break easily, thus occasionally spilling blood volume large enough to fill up the eye. This occurrence, although less common than background diabetic eye disease, is more likely to result in total vision loss especially if the patient does not receive proper intervention. If caught quick enough laser therapy can help to treat proliferative diabetic eye disease and save a patient’s vision. However, this can only be done and known to be done, if and when a diabetic person schedules regular eye exams with their doctor. Proper intervention includes but are not limited to: laser treatments and intraocular injection. These interventions along with proper control of blood sugar with primary care providers, can halt the progression of diabetic disease in the eye and may prevent devastating eye vision loss. This is why it is important for diabetic patients to get regular eye exams as symptoms can vary to each case and patient. These issues, and others that are diabetic related, can damage and blind your eyes without visible symptoms. As a precaution, the doctors here at Pisacano Eye recommend you have an eye exam on a regular basis to ensure their health.

CATARACT
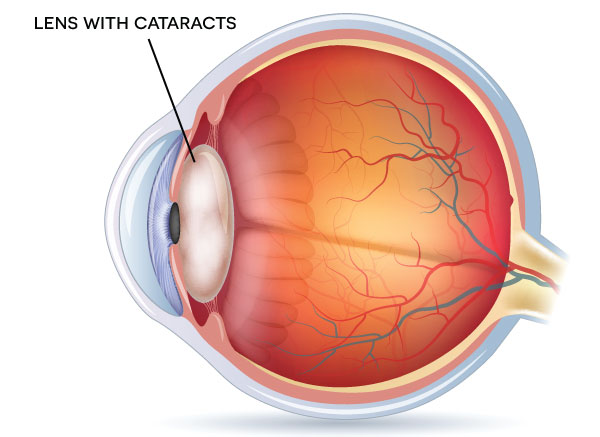
The lens of your eye is responsible for changing focus from close up to far away. It changes shape in order to bring about clearer vision. By early 40s, most people lose the ability to see up close and require bifocals or reading glasses. This is due to the fact that this lens hardens over time and is unable to change its shape. More than one glasses prescription is usually prescribed so people can see close up and far away in later years of life.
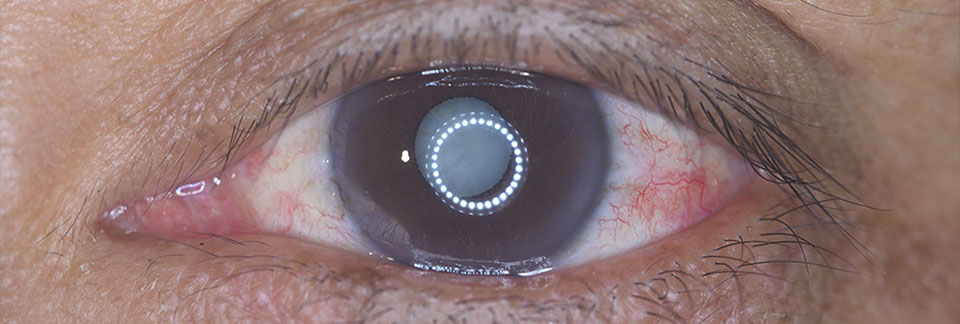
A cataract is when our natural lens in our eye becomes cloudy. It can be due to age (most common cause), injury, diabetes, steroid use, congenital.
Symptoms: Cataracts can produce an array of symptoms which include but are not limited to:
- Eyes that aren’t in the right position (misaligned)
- Rhythmic eye movements that can't be controlled (called nystagmus). The eyes may go back and forth, up and down, around, or mixed.
- Cloudy or blurry vision
- Trouble seeing
- Lights that look too bright or have a glare
- Seeing a circle of light around an object (halo)
Cataracts can be diagnosed with a visual acuity test and pupil dilation.
Treatment:
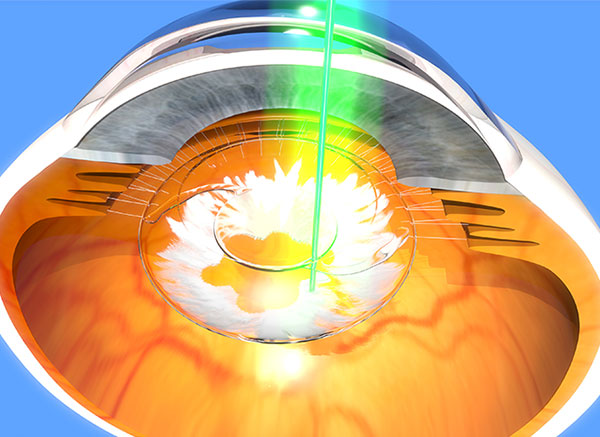
The only way to definitively treat cataracts is through surgery. Today’s modern cataract surgery is an out-patient procedure, taking 30 minutes or less, that allows patients to get back to normal activities within a few days. This is due in part to the fact that modern cataract surgery uses a variety of state-of-the-art technical equipment and techniques.
One of the most notable advancements in cataract surgery to date involves the use of topical anesthesia before surgery. Gone are the days of having to be put to sleep for this procedure. In addition to topical anesthesia, a few numbing droplets are placed on the eye. The combination of this method eliminates the risk and discomfort of the previously used shot behind the eye.
The technique to remove cataracts has also improved with time. Modern cataract surgery is performed with a small incision, less than 1/8 of an inch long. It previously use to be over ½ of an inch. After the tiny incision is made a very small instrument is inserted and breaks up theh cataract into smaller pieces that are then removed. There are multiple advantages to this smaller incision, including a smaller rick of infection, a quicker healing time, a reduced need for glasses, and the lack of stitches needed to be used.
During surgery, the cloudy lens of the eye is replaced with a lens implant. Since modern medicine has evolved, there exists various types of implants. These implants are available to correct different types of refractive problems which include near vision, distance vision, and even astigmatism. These implants may reduce the need for any type of glasses, even reading glasses, after the surgery is complete.
Nowadays, cataract surgery is one of the most successful operations performed in medicine. However, like with any surgery, there are still risks such as swelling, inflammation, bleeding, retinal detachment. The most severe risk is developing an infection known as endophthalmitis. To reduce the chances of developing this infection, your eye doctor will prescribe antibiotics for you to use after the surgery.

Before cataract surgery, the doctors here at PIsacano Eye will measure your lens strength in order to determine what replacement lens will fit best. If you wear glasses, this lens strength could replace both your current lens and your need for glasses. Like the aged lens prior to surgery, this replacement lens cannot change its shape. However, options are available to help minimize or remove the need for glasses after surgery. As an example, the lens you may be given will help see at a distance, but reading glasses may still be needed for up-close vision.
Sometimes the doctor will fit one eye with a lens meant for distance vision and the other for close up vision, this way the patient can see clearly at all distances. This does not always work well for some, as an issue with depth perception may arise.
More recently, bifocal and multifocal lenes have been created. Multiple manufacturers now have lens implants available that have been FDA approved. For those interested in the most recent lens technologies, we encourage you to discuss this with your eye doctor during your visit. The price tag on newer technologies is often expensive and considered an elective by insurance companies. Please talk to your insurance before the procedure to see if the cost for these implants will be paid out of pocket.
GLAUCOMA

Glaucoma is a group of eye conditions that damage the optic nerve involving intraocular pressure that can lead to blindness if not treated. Glaucoma is a disease that is difficult to quantify at times since what is most commonly affected is one’s peripheral vision in contrast to central vision. Peripheral vision is hard to assess, thus is it important to have scheduled regular follow-up appointments as a spectrum of exams are warranted in order to assess the disease. There are many different causes and types of glaucoma, however, it most often involves elevated intraocular pressure. Elevated eye pressure is due to a buildup of a fluid (aqueous humor) that flows throughout the inside of your eye. This internal fluid normally drains out through a tissue called the trabecular meshwork at the angle where the iris and cornea meet. When fluid is overproduced or the drainage system doesn't work properly, the fluid can't flow out at its normal rate and eye pressure increases.
Glaucoma tends to run in families. In some people, scientists have identified genes related to high eye pressure and optic nerve damage.
Risk factors:
Because chronic forms of glaucoma can destroy vision before any signs or symptoms are apparent, be aware of these risk factors:
- Having high internal eye pressure (intraocular pressure)
- Being over age 60
- Being black, Asian or Hispanic
- Having a family history of glaucoma
- Having certain medical conditions, such as diabetes, heart disease, high blood pressure and sickle cell anemia
- Having corneas that are thin in the center
- Being extremely nearsighted or farsighted
- Having had an eye injury or certain types of eye surgery
- Taking corticosteroid medications, especially eyedrops, for a long time
Symptoms:
Glaucoma has no distinct features. It is often labeled as “a silent disease” as the progression of the disease can be very slow and unnoticeable. Some symptoms, although not common, can include constant eye pain, pressure sensation, headaches, rainbow-colored halos (especially around lights), vision changes (low vision, blurred vision, tunnel vision, or blind spots).
What is a glaucoma visit:
During these visits, the doctor will ensure that your glaucoma is not progressing too rapidly getting worse by performing a number of tests to check your vision, how well you see peripherally, and the measurement of your intraocular pressure. At every visit, our doctors perform tests to check the pressure in your eyes. This is due to the belief that high eye pressure plays a role in the destruction of vision. We have several ways to measure eye pressure, including an air puff test and a blue light test.
Our doctors may also measure the thickness of your cornea. The thickness of this clear window covering in the front of your eye may affect the measurements of your eye pressure tests. Knowing how thick your cornea is can help your doctor to determine the stage of glaucoma you are experiencing, how to control it better, and any needed treatment adjustments.
Often our doctors will dilate the pupil during our eye exams to better observe the optic nerves. These nerves are what become damaged in glaucoma. When it is damaged, a person slowly loses peripheral vision. There are also computerized optic nerve scans available. This examination, in culmination with the other two, helps assess the stage of your glaucoma.
As glaucoma destroys peripheral vision, every so often our eye doctor may ask you to take a visual field test to assess your peripheral vision. This test requires a small light appearing in different areas of your peripheral vision. It allows your eye doctor to assess where it remains. If your peripheral vision continues to dissipate, your eye doctor will change your treatment.
All of these tests are necessary to ensure the health of your eyes and keep track of your glaucoma’s development. Keeping your appointments regularly and using the eye drop medication as prescribed will help keep the glaucoma under control and ultimately save your sight.
Treatment:
Glaucoma can lead to blindness if left untreated. The eye naturally is filled with a clear fluid that flows through a spigot and then out through a drain. With glaucoma, the drain of the eye is plugged and the fluid is unable to leave, causing the pressure in the eye to rise. Ultimately the pressure in the eye causes nerve damage and causes vision loss.
There is currently no cure for glaucoma, however, there are several effective treatments that can slow down the progression of the disease.that can improve a person’s sight. Successful glaucoma treatment, through medicated eye drops, ultimately lowers eye pressure.
Alternative interventions can include minimally invasive glaucoma surgeries, laser treatments, and medication pills.
Another way to lower eye pressure is through laser therapy. The type of laser therapy used on glaucoma patients is called selective laser trabeculoplasty, or SLT. SLT involves laser therapy on the drain of the eye to open it up and let more fluid out, lowering eye pressure. This therapy is performed in the office and not in an operating room. It is safe and effective for most people. The treatment is FDA approved and covered by nearly all insurance plans.
Are You an SLT Candidate?
The following descriptions below are for those who may benefit from SLT. Please feel free to ask one of our doctors at your next appointment about SLT.
- Eye pressure is uncontrolled despite the use of one or more eye drop medications.
- An inability to tolerate eye drop medications whether from medical conditions or allergies
- An inability to physical put eye drops in your eyes, such as arthritis, tremors or poor vision.
- Forgetting frequently to use your eye drop medication
- An inability to afford the cost of eye drop medication
- A desire to reduce the number of medications being used to treat glaucoma
- A desire to avoid starting use of eye drop medications to treat glaucoma, for those recently diagnosed.
Prevention:
Prevention is key when it comes to glaucoma intervention. Some things Pisacno recommends are as follows:
- Regular dilated eye examinations
- Know your family eye health’s history
- Take prescription eye-drops regularly
- Wear eye protection
CORNEA
COMING SOON
LASIK

Refractive surgery refers to any surgery performed to reduce or eliminate the need for glasses or contact lenses. All types of surgery are meant to address myopia, hyperopia or astigmatism issues.
Myopia, or nearsightedness, is when a person can see things clearly up close but struggles to see things at a distance. Myopia occurs when the cornea of the eye is steeper than average. Hyperopia, or farsightedness, is when a person cannot see well close up or far away. The cornea for those with hyperopia is flatter than usual. Astigmatism is a mixture of the two previous conditions and is characterized by a saddle shaped cornea.
Refractive surgeries help to improve the focusing power of the eye. To do this, eye doctors will alter the two main components of the focusing system, either the cornea or the lens.
LASIK:
What is LASIK surgery?
LASIK eye surgery is the best known and most commonly performed laser refractive surgery to correct vision problems
ADVANCES:
There are many advances in technology for refractive surgery that have improved the success of the procedure. These surgeries ultimately reduce the need for glasses or contact lenses. Whether you suffer from nearsightedness (myopia), farsightedness (hyperopia), or an astigmatism, refractive surgery can may help. All of these issues stem from a general issue with the eye’s focusing system, whether it be too weak or too strong. Refractive surgery will correct these issues so the patient can see clearly.
LASIK is the most common and most well-known refractive surgery. During this procedure, a corneal flap is cut from the front surface of the eye and folded out of the way a laser sculpts the corneal shape to fit your specific needs. The flap is then repositioned and the procedure is complete. A new laser, a femtolaser, was developed to create this corneal flap without the use of a blade, allowing for a more precise flap and more control over the size, shape and thickness. This in turn leads to an even higher quality of improvement in vision.
LASIK is very successful; however, some patients do develop unwanted visual effects such as glares, reduced contract or halos. These stem from errors in the eye’s focusing system, known as higher order aberrations. These issues can now be measured using wavefront analysis. Between this new wavefront analysis and the most precise lasers created, patients can enjoy visual clearness from LASIK without the problems of glares, halos or contrast sensitivity.
LASIK involves using a laser to reshape the cornea by sculpting a patients prescription into their eye. To avoid soreness, doctor’s fold away a small layer of the cornea while performing this surgery and then return it once they have finished sculpting. The procedure is nearly painless, extremely successful and the visual improvements can be seen immediately.
A secondary surgery known as LASEK is used with a thinner flap and is performed on those whose cornea is too thin or flat for LASIK. There is a third type of surgery called PRK, different from LASIK OR LASEK, in which no flap is made and a laser directly sculpts the surface of the cornea.
In addition to these refractive surgeries on the cornea, there are also two common surgeries on the lenses. One is an implantation of an ICL. This is an intraocular contact lens and essentially is a contact lens permanently placed inside your eye. The implant will rest below the surface of the eye’s natural lens, behind the iris. The strength of this lens is measured to correct the patient’s refractive error. The second procedure is known as refractive lens exchange, or RLE. This involves removing the natural lens of the eye and replacing it with an implant that corrects the refractive error.
There is another popular refractive procedure known as refractive lens exchange, or RLE. In this procedure, the natural lens of the eye is removed and replaced with a lens implant that has the perfect amount of focusing power to provide clear vision without the need for glasses or contacts. This is similar to cataract surgery, except this surgery is performed before cataracts develop. However, There is a drawback to RLE. The implant lenses only have a singular focusing power, meaning the patient will only be able to see clearly in a distance but will still require reading glasses for close up visuals. There have been developments in multifocal lenses, and we encourage you to discuss these options with your doctor as well as your insurance in advance of your surgery.
Each procedure has a benefit and a risk to it. Each is designed with a specific refractive error in mind. If you are considering having any refractive eye surgery at Pisacano Eye, we encourage you to speak to our eye doctors about your options before choosing a specific surgery.
DRY EYE

Dye Eye Disease is an eye disease that involves the imbalance of natural tear films in one’s eyes and their inability to properly lubricate the surface of one’s eyes. Tears not only provide proper lubrication, but they also are vital in the reduction of risks of eye infections, they wash away any foreign matter in our eye and maintain the eye’s surface smooth and clear. Any excess tears in our eyes flow into the small drainage system located on the corners of our eyelids. Millions of Americans suffer from dry eye syndrome. Those with this disease often feel burning or stinging in their eyes, their eyes feel sticky and are often red. Some people with this condition have periods of time when their eyes become watery and tears spill out.
Causes:
The eye’s tear film is composed of 3 different layers, each serving a different purpose. For the tear film to do its job properly, all layers must have the exact amount needed and be located in their proper places. If any layer is missing or lacking, the tear film no longer functions across the eye as it should.
Though there are multiple reasons dry eye syndrome can start, the main condition is due to abnormal or evaporating tears leaving the eye’s surface too quickly.
Symptoms:
Symptoms of this diseases include itchy, burning and scratchy sensations, similar to the feeling of having sand in your eye. Many also complain of on-and-off blurry vision that is slightly improved by blinking rapidly.
Once the eye becomes inflamed it progresses to giving the patient a stinging or burning sensation. Once the burning begins, the standard tear film is ignored and the eye creates more of the aqueous layer to soothe itself. Unfortunately, this excess of tears does not help and simply run down a person’s cheeks, taking the other two tear film layers with it. This in turn perpetuates the eye irritation and it continues like a cycle.
While this condition often seems more like an annoyance than a serious issue, if left untreated, dry eye can cause serious problems or even blindness. Inflamed eyes can lead to infection and scarring. If scarring happens, vision can be lost. We encourage those visiting Pisacano Eye to address any issues with dry eyes with our doctors so we may assess the symptoms before they develop too drastically.

This disease is often quite the nuisance to people throughout their everyday lives. In some more unfortunate cases, dry eye syndrome can lead to scarring and vision loss. Pisacano Eye offers several treatments available to help with dry eye. These can range from small lifestyle changes to prescription medication.
Those who deal with mild dry eye could potentially improve their symptoms by changing their habits. Sitting next to heating or cooling vents that our pumping out forced air can cause tears to evaporate quickly and lead to symptoms of dry eye syndrome. Humidifiers are also helpful to keep tears from evaporating, even when one isn’t sitting directly next to a heating/cooling vent. Cigarette smoke can also irritate the eyes and quitting often improves the effects of dry eyes.
There are also tear replacements available over-the-counter in most drugstores and grocery stores. Using these artificial tears in your eyes between two and four times a day can help relief the eye’s surface. The bottles sold over-the-counter are either single-dose vials or multi-dose bottles. While the multi-dose bottles are cheaper, they also contain a preservative within them that may be an irritant for some with excessive use. The single-dose vials do not contain any preservatives.
Those who tried artificial tears and noticed they used them more than four times a day may want to look into punctal plugs. The punctum is the opening of the lower eyelid where tears drain from. By plugging this drain, tears or artificial tears will stay on the eye’s surface for an extended period of time, improving dry eye symptoms. These punctal plugs can be inserted at our office quickly, easily and pain-free. Our professional eye doctors can also remove the plugs just as easily.
Those with moderate to severe symptoms of dry eye may want to discuss with our doctors about medical therapy. We can prescribe prescription eye drops to stimulate the tear glands within the eye. These eye drops can be costly, so this solution may not be for all. We encourage you to bring up your dry eye symptoms at your next visit to Pisacano Eye. Based on your conversation with our doctor, we will determine the best course of action in your treatment plan.
Dry eye syndrome has a variety of treatment options. Simple changes for those with very moderate dry eye include a change in lifestyle or habits. Do not sit close to heating or cooling vents. Invest in a humidifier to keep the air moist. Quit smoking cigarettes. There are also over-the-counter artificial tears that can help to soothe the eye throughout the day. For those with more severe dry eye symptoms, our eye doctors can place plugs in your tear ducts to keep your tears on the surface of your eye for longer. There are also prescription medications our eye doctors can prescribe to help stimulate tears.
Remember, itchy and burning eyes are not a sign of aging, but a sign of dry eye symptoms. We encourage you to discuss with your eye doctor any of these symptoms you may be having at your next visit to Pisacano Eye. We will happily create a treatment plan for you!

Getting older is the most common cause of dry eye symptoms. As you age, your eyes age with you. One of the most reccurring issues associated with aging eyes is dry eye syndrome. Women are particularly vulnerable to dry eyes due to hormonal changes that come with age. These changes often reduce tear production in the eye, leading to the dry eye sensation. Those whose eyes frequently feel itchy, scratchy or burning may be suffering from this condition. The symptoms of dry eye are often compared to the sensation of sand being caught on your eyes’ surface. In actuality, it is a deeper issue with the layer of tears on the surface of your eye evaporating too quickly, leading to dry eyes.
The symptoms of dry eye syndrome often worsen as the day goes by. What may have been a minor irritation at the start of the day is more exacerbated by the evening. Occasionally those who suffer from dry eyes, actually have eyes that water in excess. This is due to your eyes attempt to fix the situation by producing more tears. If your dry eye is caused by an issue with your tears themselves, this situation would not soothe the eye as intended, but simply continue the issue.
READING ISSUES

Our bodies change as we age. Unfortunately, that includes our quality of video. Many people experience a gradual loss of near vision as we reach our 40s. Not only is this normal, it’s also an unavoidable effect of aging known as presbyopia, or “old eyes”.
Anyone over 45 years old is familiar with the symptoms of presbyopia. Initial symptoms include feeling strain on your eyes when reading as the words appear to ‘run together’. After a short rest, you can resume reading before the symptom appears again. Over time, reading any print text becomes more difficult until, ultimately, impossible. You may notice that if you hold the print farther away from your eyes, the words will come into focus. As presbyopia progresses, you may find yourself holding the print at full arms-length and, eventually, even that is not long enough to bring the words into focus.
Since the lens of the eye is responsible for adjusting focus, the older we become, the more strain the lens experiences. As children, the lens of our eyes is ‘young’ and can quickly change its shape to accommodate between distance and near focus. Over the years, the lens becomes ‘stiff’ and can no longer easily change its shape, most commonly starting around 42 years of age.
If you are suffering from presbyopia, there is relief! Pisacano Eye can find glasses that can help bring print back into focus without holding it at arms-length. Reading glasses are necessary for up-close tasks and must be removed to see distance objects clearly. Reading glasses come in multiple strengths ranging from weaker diopters (+1.25 to +1.50) for beginning symptoms of presbyopia to stronger diopters (+2.50 to +2.75) for more progressed symptoms.
If you wear glasses for distance before presbyopia starts, bifocals may be right for you. Bifocals will have your distance prescription on top of the lens and your presbyopic reading subscriptions on the bottom of the lens. As with reading glasses, the strength of the bifocal part of the lens will have to be increased over the years. Contact Pisacano Eye and start seeing things clearly again!
FLASHES AND FLOATERS

Have you ever seen what looks like “floaters” in your vision? Tiny bits of clouded debris that is ‘floating’ around your vision and feels like a bug is flying your face? You may be experiencing a common eye condition called Floaters.
What are floaters?
The eye is filled with vitreous gel, a clear jelly that inflates the back part of the eye, similar to how water inflates a balloon. The older we get, the more the gel dissolves into a more watery form. Once enough of the vitreous gel dissolves, it pulls free of its attachments to the back of the eye, an action known as a posterior vitreous detachment. This can occur most commonly when we are in our late 50s or early 60s.
In other words, floaters are exactly what they sound like – small debris that appears when the vitreous gel separates from the back of the eyeball. The debris floats around the eye like snow in a snow globe. In more severe cases, the floaters are bigger and look ‘stringy’, like a spiderweb in your vision. The floaters will move around in your vision, including when your eyes move, so floaters do not stay in the same spot in your vision. Although floaters can be obnoxious, they are not a threat to your vision!
Another common symptom includes flashing lights in the very periphery of your vision. As the vitreous gel pulls loose from the back of the eyeball, it tugs on the lining, or retina, of the eye. As the retina is pulled, it creates the sensation of flashing lights in your vision. This symptom is indicative of a more serious ailment as the retina can rip or tear. The liquidized vitreous gel can then pass through the tear and cause the retina to come loose entirely, causing retinal detachment. If you notice sections of your vision disappearing, you may already be experiencing retinal detachment and may require surgery to repair.
If you experience any of these symptoms suddenly, call Pisacano Eye immediately for the next available appointment! Our doctors will perform an examination and determine if you are experiencing any retinal detachment. When caught early, we can send you to a specialist that can help repair your retina.
Treatment:
OCULOPLASTIC
Oculoplastic is a specialty focused on the eyelids, tear ducts, and the area around your eyes. Our Oculoplastic services can help restore comfort, function, and natural appearance when medical or cosmetic concern arise
Pisacano Web Portal
Click the button to access the Pisacano Eye Web Portal, for patient profile and medical history.
